A thrilling journey
Report of the global VR-haptic education meeting co-organised by the VR-Haptic Thinkers Team, University of Eastern Finland, and the University of Utah
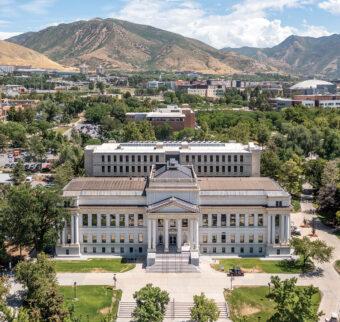
I visited the University of Utah, Salt Lake City, for the first time this summer, and I can hardly believe it took me 26 hours to get there from Finland! But I made it to the capital city of Utah, and the Mormons…
How did I get the chance to visit the Land of Mormons?
In an ever-evolving digitised world, filled with distractions, dental educators have the difficult task of teaching the new generations of students. VR-haptic training allows educators to guide students in performing dental exercises within a haptically-enhanced digital world. This can reduce the mental burden on students due to fear of failure, and they can practice on their own time and pace, even outside of regular teaching hours.

Haptic simulators offer an opportunity to practise dental procedures such as preparing cavities and placing fillings
Despite being digital, the acquired skills have been shown to transfer to the real world, giving educators more teaching tools before and during the more classical methods of practical dental education.
The second VR-Haptic Thinkers Meetup was held on 7 June at The University of Utah, Salt Lake City, Utah. It was given the theme of ‘VR-Haptic Dentistry, Pedagogy, and Curriculum Evolution’. It attracted a sizeable number of attendees from all over the world, with more than 29 different countries represented.
In recent years, new challenges and opportunities have arisen in dental education and research, which have needed to react to the rapid changes happening in VR-haptic education. The free-to-join, hybrid VR-haptic meetup featured a robust program for engaging with those of the dental community who are curious about the new technologies and developments in dental education.
I would like to thank Professor David Morton, Vice Chair of Dental and Medical Education, his team at the University of Utah for their help and our sponsors in ensuring the smooth running of our meetup. I would also like to thank Dr Rebecca Stolberg, Vice President of Allied Dental Education and Faculty Development at ADEA, Dr Gül Gülsün, Chief, Innovation, Clinical Education and Public Health at ADEA, and Dr Ophir Klein, the 100th President of the Iinternational Association of Dental Research (ADR), for attending and elevating our meet-up. In total, there were 17 presentations by dental and VR-haptics experts from around the world as well as a table set up for interaction between dental educators and professionals and major VR-haptic companies. They included a presentation from Professor Barry Quinn, an early pioneer in haptically enabled virtual reality simulation education.
The speakers advocated for the implementation of a VR-haptic research strategy and engaging with it where and whenever possible. As there is much to be done yet before VR-haptic simulation adaptation reaches its optimum levels, significant new initiatives in dental pedagogy, curriculum development and research will be set up. The consensus is that the members of the global VR-Haptic Thinkers Consortium need to be well-equipped to contribute to solving these challenges.
VR-haptics represent a shift in oral health education, complementing traditional simulation learning methods with standardised, immersive and interactive experiences. Research has shown that VR-haptics use can also reduce the mental burden of students.
Szabi Felszeghy is a Teacher at the University of Eastern Finland.
The application of virtual reality and augmented reality in Oral AND Maxillofacial Surgery

The ‘Gow-Gates’ nerve block, just distal to the maxillary second molar, at the height of the mesiolingual cusp tip of the maxillary second molar
Introduction
The use of virtual reality (VR) in dentistry has many benefits, including assessing anatomical regions, aiding in diagnosis, treatment planning and surgical treatment. The aim of VR is to utilise the cognitive, motor and mental functions of the operator in a standardised and safe manner. VR can be split into immersive and non-immersive VR. Immersive VR provides the additional element of incorporating the operator’s physical presence with 3D visualisation by using a wearable device that detects eye movements. Non-immersive VR encompasses a computer-generated experience.
Methods
Various systems used to capture dental and facial tissue (soft and hard) data for oral and maxillofacial surgery include cone-beam computed tomography (CBCT), laser scanner, structured light scanner and stereophotogrammetry. Existing literature from 2009 to 2019 relating to the application of VR in oral and maxillofacial surgery were analysed. More than 100 articles, comprising of eight systematic reviews, four expert reviews, nine case reports, five retrospective surveys, two historical perspectives, 13 manuscripts on virtual education and training, 14 on haptic training, and 41 articles on planning of orthognathic surgery were reviewed.
Clinical application
Dental implantology and orthognathic surgery are currently the most common use of VR in dentistry. The preoperative CBCT assessment is used to determine implant size, position, direction and proximity to vital structures. This is then relayed in surgery via a static guide approach using computer-aided-design/computer-aided-manufacturing (CAD/CAM) to enable the insertion of the implant. Accuracy levels are high at an overall navigation error of 0.35mm. Some limitations of CBCT in the assessment stage include poor contrast of soft tissues and image artefacts such as streaking and distortion. To combat this, fusion of images using CBCT and intra-oral scans are used to ensure an accuracy of within 0.5mm in cases such as orthognathic surgery planning.
Surgical training
Self-assessment is one of the many benefits of the use of VR in surgical training. Twenty one dental surgeons performed a range of case studies using haptic-enabled digital analysis with results showing reduction in errors in cephalometric analysis and more feasible landmarking. Local anaesthesia administration is also a skill that can be practised using 3D hepatic dental injections as seen in the above picture which shows a VR system for inferior alveolar nerve block injections.
Conclusion
In summary, VR has facilitated in the advancements of oral and maxillofacial surgery. Currently, most randomised studies focus on technical skills of surgical trainees and there are insufficient studies to assess the impact of VR compared to standard methods of delivering education. It can be agreed that VR offers significant potential in surgical planning and cognitive development. Integration of VR and augmented reality holds substantial benefits to improving quality of patient care and supplementation into curriculum is valuable.
Author
Keerusha Nagaendran, University of Sheffield
Tags: Conference, Haptics, technology, Travel, VR

You must be logged in to post a comment.