Low-stress alternatives
When resin-based composite is cured it shrinks by a factor of between 2 to 4 per cent depending on the product. This polymerisation shrinkage causes stresses to be incorporated in the system either within the surrounding tooth tissue, at the restoration/tooth interface or within the body of the restorative material. These stresses may lead to partial or total debond, recurrent caries, microleakage, pulpal inflammation, marginal staining, fracture or micro-fracture of the surrounding tooth or pain on chewing1-5.
Furthermore, the depth of light cure of conventional resin composite products is limited6, 7. To achieve a full curing of the resin composite, sufficient light energy of the correct wavelength of light must be provided to all of the material. In an attempt to overcome these potential problems, an incremental placement technique has long been advocated8, 9, particularly when restoring posterior teeth.
Firstly, the shrinkage which occurs with the first increment may be compensated for by the subsequent increment and so on. Secondly, it permits the dentist to place each increment such that as few walls are bonded together as possible to reduce the configuration or C factor10 in attempt to control the stresses and lastly each incremental of material may be fully cured as sufficient light may attenuate through the smaller bulk of material. This placement technique is therefore time consuming, tedious and requires meticulous technique6.
The so-called bulk fill resin composite materials have been introduced to the market in recent years with the aim of reducing polymerisation shrinkage stresses as well as simplifying and quickening the clinical placement of the material. This case report describes the successful resolution of symptoms of pain when a conventional methacrylate-based posterior resin composite material was replaced by a bulk fill restorative material.
Case report
A 35-year-old female geotech engineer with a clear medical history presented for her routine dental examination. A debonded, but still in situ, disto-occlusal resin composite in ı6 was diagnosed with no obvious caries present. An appointment was made so that the restoration could be replaced.
At the treatment appointment, a local anaesthetic was administered and rubber dam placed. The existing restoration was removed and cavity refined. As it was considered not to be deep, no lining was considered necessary. After a sectional matrix system (V Ring, Triodent) had been placed, the cavity was etched with Scotchbond Universal Etchant (3M ESPE) for 15 seconds, washed for 15 seconds and lightly air dried leaving a glassy dentine surface.
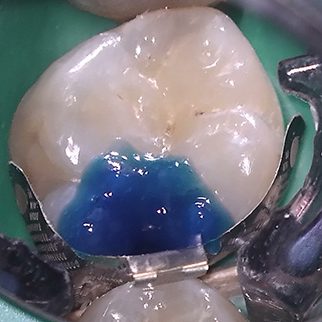
Adper Scotchbond 1XT (3M ESPE) was then applied, air thinned and cured for 20 seconds. Filtek P60 Posterior Restorative (3M ESPE) was placed into the cavity using an incremental placement technique with each increment cured for 40 seconds. The matrix system was removed and gross finishing done using diamond finishing burs (Figure 1). Once the rubber dam had been removed and the occlusion checked, the restoration was polished using rubber points.
However, the patient returned two weeks later complaining of a tenderness on biting which necessitated her avoiding using the tooth. She had some sensitivity to cold stimuli but this had settled a few days before the unscheduled appointment. Clinical examination revealed nothing untoward and so the patient was reassured but advised to return if things did not settle. Unfortunately, as the same pain on biting was persisting, she returned a fortnight later. Clinical examination revealed that ı6 was tender on application of a Tooth Slooth and when pressure was released when the tooth was squeezed. The diagnosis was therefore made of cracked cusp syndrome most likely precipitated by stresses caused by the polymerisation shrinkage of the resin composite. The patient was advised that the restoration should be replaced in an attempt to remove any stresses within the tooth tissue.
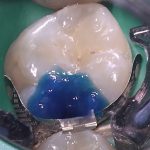
At a subsequent appointment, local anaesthetic was again administered, rubber dam placed and the restoration removed (Figure 2). A sectional matrix system (V Ring, Triodent) was placed, the cavity was etched with Scotchbond Universal Etchant (3M ESPE) for 15 seconds (Figure 3).
The etchant was washed using water from the three-in-one syringe for 15 seconds and lightly air dried leaving a glassy dentine surface. Adper Scotchbond 1XT (3M ESPE) was applied, air thinned and cured for 20 seconds. As before, no lining was considered necessary as the bonding agent would seal the dentinal tubules. Filtek Bulk Fill Posterior (3M ESPE) was placed into the cavity in a single increment, contoured before being light cured for 40 seconds (Figure 4).
The restoration was grossly finished using diamond finishing burs after the sectional matrix had been removed (Figures 5 and 6). The rubber dam was removed, the occlusion checked and the restoration finished and polished (Figure 7).
- Fig 1 – 16 DO cavity restored with Filtek P60 Posterior Restorative (3M ESPE) after gross finishing but before the rubber dam had been removed
- Fig 2 – The completed cavity after the restoration had been removed
- Fig 3 – A V Ring (Triodent) sectional matrix placed and the cavity etched with Scotchbond Universal Etchant (3M ESPE)
- Fig 4 – Filtek Bulk Fill Posterior (3M ESPE) after light curing
- Fig 5 – Filtek Bulk Fill Posterior (3M ESPE) after light curing
- Fig 6 – A higher magnification photograph, note the good contact area
- Fig 7 – The completed 16DO Filtek Bulk Fill Posterior (3M ESPE)
The patient was reviewed at her routine six-monthly dental examination four months later. She had no complaints as the symptoms of pain had resolved completely and very quickly after the appointment to replace the conventional posterior resin composite restoration with the bulk fill product. The patient has been reviewed for her routine dental examination six months subsequent to this and the tooth remains asymptomatic and signless.
Discussion
This case is interesting as, in many respects, direct comparison may be made between both the original appointment and the subsequent remedial appointment as the procedure performed was largely identical. The operator, the method of anaesthesia, timing and placement of rubber dam, burs, sectional matrix system, etch, bonding agent and method and instruments used to finish the restoration were the same at both appointments.
The only differences were that a bulk fill product was used instead of a conventional posterior resin composite and the former product was placed in one increment by definition. The placement of the conventional resin composite could be viewed as a “control” and a direct means of comparison to the new bulk fill product.
It is known that stresses may be incorporated into the system as a result of polymerisation shrinkage which occurs when the resin composite is cured ı. In this case, these stresses had precipitated signs and symptoms of incomplete fracture of the tooth structure (cracked cusp syndrome) despite its meticulous placement in the first instance. Bulk fill resin composites were developed to reduce these stresses and simplify and so quicken their clinical placement. This due to the manufacturer making modifications to the constituents of the material.
In the case of the product used in this case, BisGMA (the most commonly used monomer in resin composite products) has been omitted in favour of other monomers such as ERGP-DMA, urethane dimethacrylate (UDMA) or 1,12-Dodecane dimethacrylate (DDDMA)11.
UDMA is relatively low-viscosity, high-molecular weight monomer which means that there are fewer reactive groups and so the volumetric shrinkage is minimised. Furthermore, the stiffness of developing and final polymer matrix is decreased but a tough, highly cross-linked network is still created.
DDDMA provides a high-modulus resin with good flexibility and impact resistance. This monomer cures quickly and exhibits a low exotherm and low shrinkage. The omission of BisGMA means that bisphenol A is, by definition, absent following concerns over its potentially oestrogenic side effects such as breast and prostatic carcinomas and male infertility. Two other monomers have been incorporated in the resin system which work in combination to reduce polymerisation stresses11. One is a high molecular weight aromatic dimethacrylate (AUDMA) with a reduced number of reactive groups. This moderates the volumetric shrinkage and the stiffness of the developing and final polymer matrix.
Another class of compounds called addition-fragmentation monomers (AFM) work in combination with AUDMA to decrease the shrinkage stress. These methacrylate molecules react into the developing polymer by forming crosslinks between adjacent polymer chains. When stressed during polymerisation, these molecules may break or fragment so providing a means for relaxation of the developing polymer network and so stresses are relieved.
These fragments also react with each other or other nearby reactive sites in a less stressed environment as the polymer develops. This process goes to completion maintaining the physical properties of the polymer as the conversation is the same but with greatly reduced polymerisation stress. This was well illustrated in the present case with almost immediate resolution of the patient’s symptoms of pain.
The bulk fill product was placed in one increment as the cavity was shallower than 4mm. To enable light to fully penetrate through the material to permit an increased depth of cure, the manufacturers may utilise three strategies to achieve this:
1. Lower the filler content and/or increase the filler particle size
2. Modify the resin to increase its translucency
3. Use a different photoinitiator system.
The filler used in Filtek Bulk Fill Posterior (3M ESPE) is a silicon/zirconia nanofiller which conveys good wear resistance, increased strength, excellent polish retention and favourable handling. The total inorganic filler loading of approximately 76.5 per cent by weight (58.4 per cent by volume)11. This may be compared to the filler loading of a flowable resin composite which is approximately 65 per cent
by weight.
This means that the second generation of bulk fill products of which Filtek Bulk Fill Posterior (3M ESPE) is an example, can be used to restore the entire cavity without the need for a veneering layer using a resin composite indicated for use in the posterior region which is necessary with the lower viscosity products12 as they have inferior mechanical properties due to their lower filler loading. Due to other modifications in the chemistry of the material discussed elsewhere in this paper, the higher filler load has been possible without any detrimental effect on light attenuation.
Bulk fill materials tend to be more translucent to permit increased light attenuation through its mass. The manufacturer of the product used in the present case describes the material as semi-translucent11.
As can be seen in Figure 7, the aesthetics of the cured material are acceptable but a slight mismatch in shade is evident between the resin composite and tooth tissue.
This is considered advantageous by many clinicians because, if the restoration requires to be subsequently removed, the tooth tissue may be more easily identifiable and so may be preserved6.
Many of the bulk fill products available on the market use photoinitiators which have a higher visible light absorption rate which allows increased quantum efficiency. In simple terms, this
means that a lower quantity of light (photons) is required to trigger the polymerisation free radical chain reaction. This results in improved light-curing performance and an increase depth of cure.
These modifications to the chemistry of this product have allowed the placement of Filtek BulkFill Posterior (3M ESPE) in one increment which greatly simplified and quickened the clinical procedure.
Conclusion
This case illustrates that an alternative low-stress material (so-called bulk fill) may successful resolve symptoms caused by polymerisation stresses when conventional resin composite is cured as it exhibits markedly reduced polymerisation stresses.
Consideration should be given to selecting one of these bulk fill materials in preference to a conventional posterior resin composite material when working in the posterior region of the mouth, not only in terms of stress reduction but the clinical procedure is simpler and quicker.
Conflict of interest/commercial interests
The author denies any commercial interest in any of the dental products or dental companies mentioned in this paper.
About the author
Mr Steve Bonsor BDS(Hons) MSc FHEA FDS RCPS(Glasg), is a GDP and practice principal at The Dental Practice in Aberdeen. He graduated from the University of Edinburgh in 1992 and gained aDiploma in Postgraduate Dental Studies from the University of Bristol and completed a MSc at the same university in 2008.
He has previously held posts as a clinical teacher at Dundee Dental Hospital and School and honorary clinical teacher at the University of Dundee in the sections of operative dentistry, fixed prosthodontics, endodontology and integrated oral care.
Steve currently holds appointments at the University of Edinburgh as an online tutor on the MSc in Primary Dental Care programme and at the University of Aberdeen as honorary senior clinical lecturer and senior clinical teaching fellow leading the applied dental materials teaching at Aberdeen Dental School. In addition, he is heavily involved in postgraduate dental education having lectured throughout the UK.
To contact Steve, email steve.b@thedentalpracticeaberdeen.co.uk
References
1. Davidson CL, de Gee AJ, Feilzer A. The competition between the composite-dentin bond strength and the polymerization contraction stress.
J Dent Res 1984 Dec;63(12):1396-1399.
2. Davidson CL, Feilzer AJ. Polymerization shrinkage and polymerization shrinkage stress in polymer-based restoratives. J Dent 1997 Nov;25(6):435-440.
3. Letzel H. Survival rates and reasons for failure of posterior composite restorations in multicentre clinical trial. J Dent 1989;17 Suppl 1:S10-7; discussion S26-8.
4. Tantbirojn D, Versluis A, Pintado MR, DeLong R, Douglas WH. Tooth deformation patterns in molars after composite restoration. Dent Mater
2004 Jul;20(6):535-542.
5. Loguercio AD, Reis A, Schroeder M, Balducci I, Versluis A, Ballester RY. Polymerization shrinkage: effects of boundary conditions and filling technique of resin composite restorations. J Dent 2004 Aug;32(6):459-470.
6. Bonsor SJ, Pearson GJ. A Clinical Guide to Applied Dental Materials. 1st ed. Edinburgh: Churchill Livingstone Elsevier; 2013.
7. Yap AU. Effectiveness of polymerization in composite restoratives claiming bulk placement: impact of cavity depth and exposure time. Oper Dent 2000 Mar-Apr;25(2):113-120.
8. Lee MR, Cho BH, Son HH, Um CM, Lee IB. Influence of cavity dimension and restoration methods on the cusp deflection of premolars in composite restoration. Dent Mater 2007 Mar;23(3):288-295.
9. Poskus LT, Placido E, Cardoso PE. Influence of adhesive system and placement technique on microleakage of resin-based composite restorations. J Adhes Dent 2004 Autumn;6(3):227-232.
10. Feilzer AJ, De Gee AJ, Davidson CL. Setting stress in composite resin in relation to configuration of the restoration. J Dent Res 1987 Nov;66(11):1636-1639.
11. 3M ESPE. Filtek Bulk Fill Posterior Restorative Technical Product Profile.
12. Burgess J, Cakir D. Comparative properties of low-shrinkage composite resins. Compend Contin Educ Dent 2010 May;31 Spec No 2:10-15.






You must be logged in to post a comment.