Aesthetic orthodontic brackets Are they all the same?
Preet Bhogal compares and contrasts the advantages and disadvantages of various aesthetic labial brackets on the market
History of aesthetic brackets
The last 30 years in particular have seen an increasing need to produce an aesthetic, well-hidden camouflaged labial bracket that is acceptable to the discerning patient. With the recent increase in demand for orthodontic treatment, this essential requirement has been stressed further by dentists and patients alike.
It is important to learn from the abundant research that has already been carried out in order to avoid using poor materials and provide evidence-based treatments for our patients.
Orthodontic brackets can be classified by material type (metal, plastic, composite and ceramic), shape (siamese, self-ligating) and slot size (0.022” x 0.028” or 0.018” x 0.028” most commonly).
We will not be considering metal brackets here, which are made of stainless steel alloy. Modern ceramic bracket technology has developed significantly since the mid-1980s.
The aim of this article is to compare the properties of various types of aesthetic labial brackets available and highlight their relative advantages and disadvantages. It is important that the clinician chooses the best available materials for clinical use and is able to distinguish between high and low-quality materials. All the various types of brackets have been previously tried and tested by numerous researchers.
You should ask yourself the following questions about the brackets you use:
- What is the prescription?
- What material are they made of?
- What is the design of the base?
- What is the bond strength?
- Have they been tested for quality?
- How rigorous is this quality control?
- Would you be comfortable using your current materials after reading this review?
- Are they actually value for money?
- Which ones would you use on yourself or a family member?
Bracket prescriptions
It is the interaction of the orthodontic bracket and the archwire that controls tooth movement. The relation of one to another can be manipulated to produce desired movements in all planes of space. The size and properties of each can also be altered to change how forces between the two are transmitted.
The bracket slot size in straightwire fixed appliances is most commonly 0.022” x 0.028” as this allows for lighter forces in the early stages of treatment and is good for archform co-ordination and sliding mechanics.
The first straightwire brackets were essentially composed of a horizontal slot (in which the archwire sits) passing through a twin (or Siamese) bracket. All tooth movements were effected via the orthodontist skill and required great technical ability in wire bending.
Pre-adjusted brackets have in-built values that predetermine tooth movements and are specific for each tooth or tooth group. Essentially, they have a “prescription” for 1st, 2nd and 3rd order bends, or putting it another way values for in-out, tip and torque (Fig 1).
The most common pre-adjusted bracket prescriptions used by orthodontists worldwide are:
- Andrews
- Roth
- MBT
- Damon.
Each of these have their own justifications based on the approach and research of their developers, all of whom are/were esteemed orthodontists and based on observations of large numbers of treated cases.
The benefit of a well-known and tested prescription (such as those listed) that has been rigorously tested and proven is obvious. As a prescribing dentist, you would be expected to have knowledge of (and therefore use) a tested and widely accepted appliance prescription. For those simple cases that may run into difficulty and necessitate transfer or referral, using an established bracket system enables the receiving orthodontist to pick up the case with a knowledge of where the teeth have been pre-programmed to move. It is unlikely therefore that spurious brackets will have to be removed and then re-bonded with known and proven ones. This will save time, money and discomfort/potential enamel damage to the patient.
Ideal properties of an aesthetic bracket
These can be broadly divided into:
- optimum aesthetics
- optimal clinical performance.
The first point is rather obvious but there are discernible differences according to quality. The second point requires further understanding and elaborating upon. We will discuss each type of aesthetic bracket in turn.
Plastic brackets
Plastic brackets were introduced in the 1970s. Initially, they were made from acrylic or polycarbonate. Problems were quickly identified, including staining and odours1. More importantly, their lack of strength and stiffness resulted in bonding problems, tie wing fractures and permanent deformation2. Their success, as a viable alternative to metal brackets was understandably short lived. Plastic bracket slots distort with time under a constant stress, rendering them insufficiently strong3. Also, and importantly, much of the energy stored in the aligning archwire was expended in distorting the brackets due to the poor integrity of the bracket slot and therefore archwire forces were not transmitted effectively for tooth movement. A comparison with stainless steel brackets illustrated that plastic brackets are only suited for clinical application if they have a metal slot1 (Fig 2).
Composite (thermoplasticpolyurethane)
To compensate for the lack of strength and rigidity of the original polycarbonate brackets, high-grade medical polyurethane brackets reinforced with ceramic or fibreglass fillers and/or metal slots were introduced1. Brackets with metal reinforced slots demonstrated less enamel wear than ceramic and significantly less creep than conventional plastic polycarbonate brackets, although initial problems still existed (Fig 3).
Ceramic brackets
Ceramic brackets were introduced in the 1980s, offering several advantages over the aforementioned aesthetic brackets:
- higher strength
- greater resistance to wear and deformation
- better colour stability
- superior aesthetics.
All currently available ceramic brackets are composed of aluminium oxide (alumina) in either polycrystalline or monocrystalline form, depending on their method of fabrication.
The first brackets were each milled from a single crystal of sapphire and were more translucent. More recent monocrystalline brackets are machined from extrusions of synthetic sapphire and are virtually clear4.
Polycrystalline alumina brackets are made by injection moulding of submicron-sized particles of alumina suspended in a resin, sintering them to fuse the alumina and produce a bracket that is finally machined to shape5. Polycrystalline ceramics, due to their rougher more porous surface, have a high coefficient of friction. This problem has largely been overcome by the use of metal reinforced archwire slots and improvement in modern ceramic technology.
These disadvantages are not associated with simple alignment cases and non-extraction cases, where sliding mechanics is less of a requirement. More recent injection moulded microcrystalline brackets (e.g. Gemini Clear) demonstrate excellent aesthetics and are smoother, smaller, better contoured (thus more comfortable and better adapted to tooth surfaces) and stronger than conventional ceramic brackets (Fig 4).
Bond strength
The majority of currently available ceramic brackets rely solely on mechanical retention, using standard light or chemically cured adhesives, without the need for additional special bonding agents such as silane. Addition of a silane component has proved to increase the bond strength to an undesirably high level, risking enamel damage on debond. The bond strength achieved with mechanical retention alone favours a simple bonding technique. An initial pumicing of the teeth followed by self-etch primer (3M Unitek Transbond SEP) and orthodontic composite (3M Unitek Transbond APC or XT) ensures reliable bond strength when compared to cheaper quality brackets and acid-etch bonding methods. There are also significant advantages in time, labour and materials costs when compared to separate etch and bonding techniques.
Bracket bases
The subject of bracket base is very important, yet often overlooked. Several developments have occurred in modifying the bracket base design in order to reduce bond failure and achieve reliable debonding at the end of a course of orthodontics. Predictable debonding is just as important (if not more so) than predictable bonding of orthodontic brackets and should be considered/planned from the outset.
The challenge is to achieve adequate bond strength for clinical application that will not harm the enamel surface on bracket removal at the end of treatment. With this in mind, the type of bracket base is more relevant than base size. Bracket base area and bond strength have no direct relationship6. Various types of mechanical bracket base include:
- microcrystalline
- perforated
- mesh
- undercut channels
- polymer coated
- spherically photoetched
- metal/ceramic
- dovetail
- dimpled.
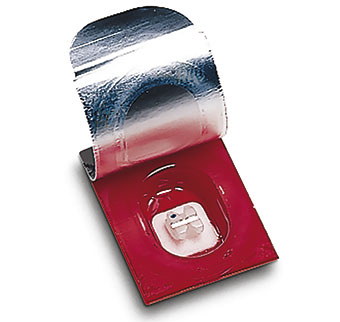
The features of the bracket base should be undisturbed/unmodified for optimum performance (Fig 5).
Debonding aesthetic brackets
The brittleness of cheap brackets can cause problems during treatment and at debond. Their hard nature can cause abrasion to the dentition and significant enamel wear has been found on the surfaces of upper incisors from contact with the lower labially placed brackets after only six weeks7. This can be reduced by the use of bite stops placed on the posterior molars (generally), to avoid occlusal contacts whilst the teeth level and align, and checking for occlusal contacts between brackets and opposing enamel. These brackets should also be avoided in deep bite cases.
A common cause of fractured brackets is scratching them with a probe/instrument/ligatures unnecessarily as this introduces micro-crazing and introduction of surface flaws. Metal ligatures should be used carefully and care taken with removal of these (unwind the metal ties).
High quality ceramic brackets can overcome the problems with fracture at debond with the use of specially designed bases to overcome these issues. The incorporation of a vertical stress concentrator ensures reliable debonding at the bracket/composite interface, leaving a layer of composite on the tooth surface. This composite can then be easily removed, protecting the enamel surface.
The procedure for debonding these brackets by “squeezing” in a mesiodistal plane is more reliable for the operator and comfortable for the patient. Uncontrolled debonding on the other hand can be very unpleasant due to the high potential of bracket fracture and teeth moving within their sockets. This can cause severe distress to the patient and undermine a healthy dentist-patient relationship. Also, grinding of a layer of fragmented bracket on the tooth surface will often generate significant heat that can cause pulpal damage and is best avoided (Fig 6).
Some tips to help the debonding procedure
- Bond strength is greatest at the bracket-composite interface and therefore enamel fracture is highly likely. A “plane of cleavage” can act as a stress breaker for comfortable debonding
- Silane coupling is not required for bonding brackets due to the quality of mechanical retention inherent in quality bracket bases. Mechanical retention reduces enamel detachment but maintains high strength, durability and retention similar to metal brackets8
- Use a weaker orthodontic-specific unfilled resin bonding agent (not a restorative bonding agent) as the brackets are supposed to be removed at a later date and a permanent bond is not required
- Use ceramic bracket with a notched pre-stressed base and plane of cleavage for debond9
- Bond with resin modified glass ionomer cement
- Remove composite flash around the brackets before debonding10
- Use the manufacturer’s debonding instruments11
Figures
Fig 1 Diagram of (a) 1st Order (in-out), (b) 2nd Order (tip) and (c) 3rd Order (torque) movements
Fig 2 Plastic bracket
Fig 3 Composite brackets
Fig 4 Microcrystalline Gemini Clear Ceramic Bracket
Fig 5 Bracket base features for mechanical retention: (a) compound contoured base, (b) microcrystalline bonding surface, (c) vertical stress concentrator
Fig 6 Gingival view of debonding a 3M ceramic bracket using a custom debonding instrument
References
1. Russell JS. Aesthetic Orthodontic Brackets. Journal of Orthodontics, Vol. 32, 2005, 146-163.
2. Arid JO, Durning P. Fractures of polycarbonate edgewise brackets. A clinical and SEM study. British Journal of Orthodontics, 14: 191-195.
3. Dobrin RJ, Kamel IL, Musich DR (1975). Load deformation characteristics of polycarbonate orthodontic brackets. American Journal of Orthodontics, 67: 24-33.
4. Swartz ML (1988). Ceramic brackets. Journal of Clinical Orthodontics, 22: 82-88.
5. Birnie D. Orthodontic material update. Ceramic brackets. British Journal of Orthodontics 1990;17:71-75.
6. Reynolds IR. A review of direct orthodontic bonding. British Journal of Orthodontics 1975;2:171-178.
7. Douglas JB (1989). Enamel wear caused by ceramic brackets. American Journal of Orthodontics and Dentofacial Orthopedics, 95: 96-98.
8. Wang WN, Meng CL, Tarng TH (1997). Bond strength: a comparison between chemical coated and mechanical interlock bases of ceramic and metal brackets. American Journal of Orthodontics and Dentofacial Orthopedics, 111: 374-381.
9. Larmour C J, McCabe J F, Gordon P H 1998 An ex vivo investigation into the effects of chemical solvents on the bond behaviour of ceramic orthodontic bracket. British Journal of Orthodontics 25: 35–39
10. Bishara S E, Trulove T S 1990 Comparisons of different debonding techniques for ceramic brackets: an in vitro study. Part II. Findings and clinical implications. American Journal of Orthodontics and Dentofacial Orthopedics 98: 263-273
11. Winchester LJ et al., 1992. Methods of debonding ceramic brackets, BJO 19;233-7